Please Support Talking-up Scotland at:
https://www.crowdfunder.co.uk/p/support-talking-up-scotland
Click on the above.
This is the second attempt by the Herald, based on unreliable statistical methods by the Daily Record (No surprise there) to misrepresent the level of ‘corridor care‘ in Scotland’s hospitals.
Explicit figures are not published anywhere but there’s a good proxy for corridor care and that’s 12 hour waits in A&E. By definition if you’re waiting 12 hours after triage assessment and maybe some treatment before getting a bed, that is ‘corridor care.’ A fuller AI rationale for the use of 12 hour waits, based heavily on the views of the Royal College of Medicine, Age Concern and even NHS England itself, is below.
A&E demand varies from month to month and, of course peaks in the winter months, so comparing one month, December, over the last four years is revealing.
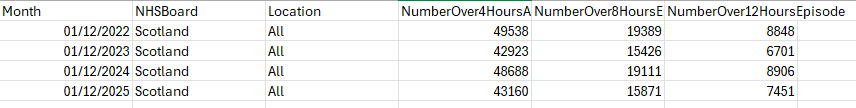
So, all A&E waits are lower than they were 4 years ago and lower than they were last year. The first media reports of ‘corridor care’ in Scotland were around July 2024. Given that A&E waits, especially 12 hour waits, are now significantly lower than in 2024, that suggest politics rather than facts.
Further, the discussion of methods below points to: In England, the key metric is 12 hours from decision to admit (most precise for corridor care). In Scotland (and sometimes advocated UK-wide), it’s often 12 hours from arrival, which includes initial assessment time and may overestimate pure corridor waits.
Sources:
Methods:
Why 12-Hour A&E Waits Are a Good Proxy for Corridor Care
Corridor care (also called trolley waits or care in temporary escalation spaces) occurs when emergency departments (EDs) are overcrowded due to a lack of inpatient beds, forcing patients who need admission to be treated in non-clinical areas like corridors, waiting rooms, or chairs. This is unsafe, undignified, and linked to patient harm.The most accurate proxy in NHS data—particularly in England—is the number of patients waiting more than 12 hours from the decision to admit (DTA) to actual admission (known as “12-hour trolley waits” or “12-hour DTA waits”). Here’s why this metric strongly indicates corridor care:
- Direct Link to Bed Availability Delays
Once a clinician decides a patient needs admission (DTA), the wait is almost entirely due to no available ward bed. Patients remain in the ED, often on trolleys in corridors or other overflow areas, receiving ongoing care there. Short DTA waits mean quick transfers to proper wards; prolonged waits (especially >12 hours) mean patients are stuck in unsuitable ED spaces. - Official and Expert Recognition
- NHS England and the Royal College of Emergency Medicine (RCEM) explicitly link these waits to corridor care. For example, NHS spokespeople have stated: “It is totally unacceptable that patients are waiting over 12 hours to be admitted to a hospital bed, and in some cases, this wait is occurring in corridors.”
- The Royal College of Nursing (RCN) describes 12-hour waits as “the clearest indicator of corridor care taking place,” since staff cannot move admitted patients to wards.
- Age UK and Liberal Democrat analyses equate 12-hour trolley waits directly with corridor care experiences.
- No Direct National Tracking of Corridor Care
The NHS does not routinely publish data on the exact number of patients treated in corridors (though some site-specific or survey data exists). In its absence, 12-hour DTA waits serve as the best available quantitative proxy, capturing the severity of exit block (delayed transfers out of ED). - Evidence of Harm and Scale
RCEM research shows long waits (8–12 hours and beyond) are associated with excess mortality (e.g., one additional death per 72 patients waiting 8–12 hours). These waits overwhelmingly occur in corridor-like settings during overcrowding.
Note on Variations in Measurement
- In England, the key metric is 12 hours from DTA (most precise for corridor care).
- In Scotland (and sometimes advocated UK-wide), it’s often 12 hours from arrival, which includes initial assessment time and may overestimate pure corridor waits.
Both are used as proxies, but DTA is more specific to the bed-delay phase where corridor care predominates.
In summary, 12-hour waits (especially DTA) reliably signal when ED overcrowding forces care into corridors, making them a vital—though imperfect—measure of this systemic issue. Experts like RCEM presidents call it a “national shame” and urge its elimination through better bed capacity and flow.
Please Support Talking-up Scotland at:
https://www.crowdfunder.co.uk/p/support-talking-up-scotland
Click on the above.